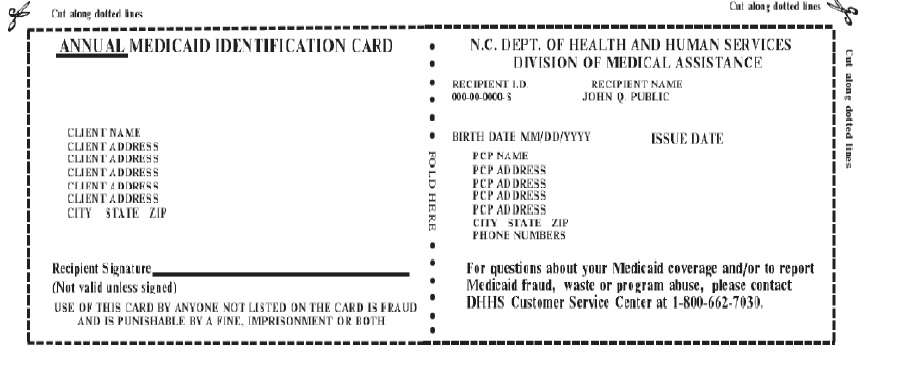
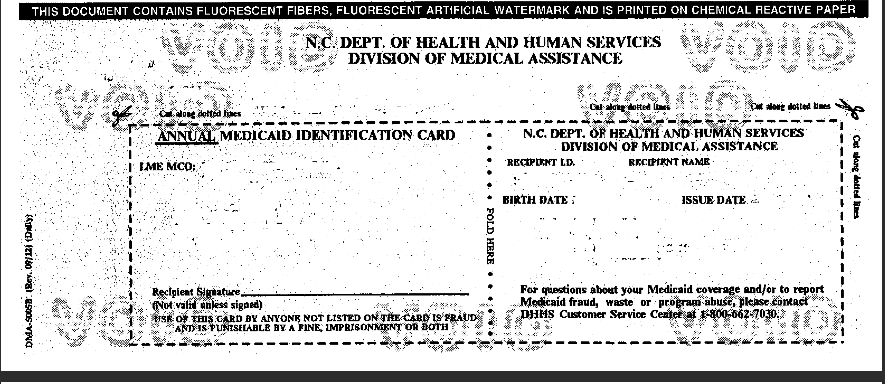
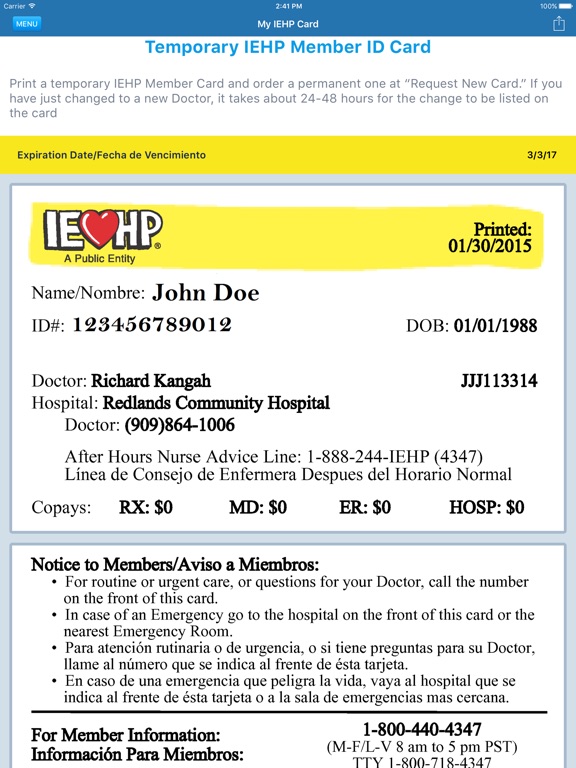
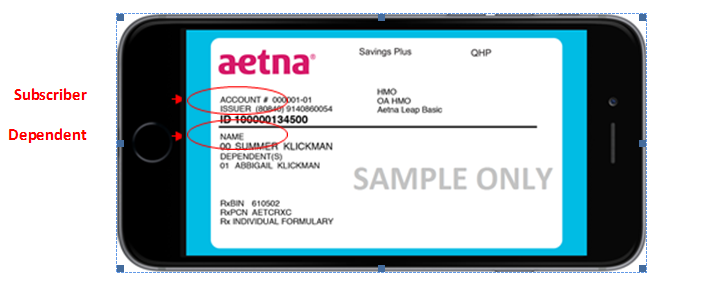
Many health insurance cards show the amount you will pay (your out-of-pocket costs) for common visits to your primary care physician , specialists, urgent care, and the emergency department. If you see two numbers, the first is your cost when you see an in-network provider, and the second—usually higher—is your cost when you see an out-of-network provider. For example, when you're referred to a specific specialist or sent to a specific hospital, they may not be in your insurer's network. Each person covered by a health insurance plan has a unique ID number that allows healthcare providers and their staff to verify coverage and arrange payment for services. It's also the number health insurers use to look up specific members and answer questions about claims and benefits. If you're the policyholder, the last two digits in your number might be 00, while others on the policy might have numbers ending in 01, 02, etc.
Your insurance company may provide out-of-area coverage through a different health care provider network. If so, the name of that network will likely be on your insurance card. This is the network you'll want to seek out if you need access to healthcare while you're away on vacation, or out of town on a business trip. The descriptions below apply to most private health insurance ID cards in the United States. If you live outside the U.S. or have government-provided insurance, you may see some different fields on your card.
When you start therapy with an Oxford Health in-network therapist, they will designate a diagnosis for your condition or goals. They'll share this diagnosis with the insurance company to ensure coverage. This is essential for coverage of your therapy sessions.
If you would prefer that your therapist doesn't disclose your diagnosis with Oxford Health, consider your out-of-network options. This way, your mental health care stays between you and your therapist -- not the insurance company and anyone who has access to your insurance account information. The cost of therapy under Oxford Health varies based on the specific plan; if you choose a provider who is in-network with your Oxford Health plan, the majority of copayments are around $50.
Because Oxford Health insurance covers more than one state, your plan will also vary by your location. All of these factors contribute to a wide range of therapy coverage. The Difference Card disrupts the healthcare status quo by helping clients create unique benefit plan designs. These plans allow you to lower your health insurance costs while maintaining a level of benefits that exceeds your company's expectations. The providers available through this application may not necessarily reflect the full extent of UnitedHealthcare's network of contracted providers.
Unitedhealthcare Oxford Policy Number On Card There may be providers or certain specialties that are not included in this application that are part of our network. We also recommend that, prior to seeing any physician, including any specialists, you call the physician's office to verify their participation status and availability. Generally, insurance companies post the Summary and Benefits document within their online portals.
If you're not able to locate this document, find the customer service number on the back of your insurance card. The customer service agent will either point you in the right direction of where to find your mental health benefits or share with you the amount of coverage you have under your plan. After going through, one can get a pretty straightforward idea about the health insurance cards. I think that it is a good idea to maintain an effective health insurance coverage.
I think that the cards should also link the patient's previous medical history. Out-of-network/non- contracted providers are under no obligation to treat UnitedHealthcare plan members, except in emergency situations. Please call our customer service number or see your Evidence of Coverage for more information, including the cost- sharing that applies to out-of-network services. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® Member Handbook.
Benefits, List of Covered Drugs, pharmacy and provider networks and/or copayments may change from time to time throughout the year and on January 1 of each year. Across the majority of Oxford Health plans, expect to pay a copayment of around $50 each therapy session for in-network providers. This means that each time that you have a therapy session, you will pay your therapist $50 out-of-pocket. Oxford Health utilizes a behavioral health program called Live and Work Well for their mental health benefits.
This program provides additional services and resources for Oxford Health participants, including information on the cost of therapy based on your plan. We encourage you to reach out to your health plan's member services department so that they may assist you with specific questions about your ID card and benefits. David joined CDPHP as a communications specialist in April 2016. He writes and edits content to support internal and external communications. David has won multiple national awards as a newspaper reporter and served as a publicist for everything from small nonprofits to global brands.
He graduated from the University at Albany with a degree in philosophy. In his spare time, David enjoys the outdoors, reading, Boston Celtics basketball, and searching for exciting and unusual experiences with uncertain outcomes. He is almost always accompanied by his children, David and Daisy. Different insurance plans sometimes cover different pharmacy networks. For example, CDPHP employer plans use a Premier network; CDPHP individual plans use a Value network; and CDPHP plans for seniors use the Medicare network. Paper copies of the network provider directory are available at no cost to members by calling the customer service number on the back of your ID card.
Non-members may download and print search results from the online directory. No, you will not need to see your primary care doctor before you see a therapist. Because the Oxford Health insurance plans are PPO and EPO plans, you do not need a referral in order to see a mental health professional. This means that it's easy to start your search for the perfect therapist and you won't have to wait before you start your therapy journey. Oxford Health is a health insurance subsidiary that falls under the UnitedHealth Care insurance umbrella, one of the largest insurers in the United States. Oxford Health is also known as UnitedHealth Care Oxford.
The majority of Oxford Health network is located in the tristate area . Oxford Health provides coverage for physical and mental health services. Below is information regarding Oxford Health insurance's mental health coverage. Health insurance policies offer numbers on the policy. According to the insurance company, you must provide the account number for tracking your medical expenses.
In the United States, a majority of the cards are insurance cards. Depending on your health plan policy or insurance card, a number signifies the coverage of that policy. You have clicked on a link to a third-party website and are leaving the BancorpSouth website. BancorpSouth does not control third-party web sites or the information, products and services offered there. BancorpSouth provides links to such sites only as a convenience and is not responsible for the privacy or security of any third-party website.
We encourage you to review the privacy policy and security offered on the third-party website prior to providing any personal information. One Medical accepts health plans from most insurance carriers as well as Medicare. Some of the more popular plans that we accept are listed here, but since the list periodically changes, we encourage you to call us if you don't see your plan. You may not think about your health insurance ID card very often.
After all, it probably spends most of its time in your wallet—until you, your doctor, or another medical provider really need it. The Wall Street Journal described their HMO as "trend-setting" and noted that Oxford "even let patients visit specialists outside its own network." As more therapists offer both in-person and online options, Oxford Health recognizes the importance of accessible mental health treatment. We are pleased to participate in a limited number of ACA/Exchange plans that enable us to provide you with the high level of care and service you expect from One Medical. Our goal is to participate with as many plans as possible, and we expect to continue to expand the list of participating plans over time.
We believe that quality health care should be accessible to everyone, so if you have a high-deductible health plan or are not insured, we also offer affordable options for working together. The Applied Behavior Analysis Medical Necessity Guide helps determine appropriate levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. The ABA Medical Necessity Guide does not constitute medical advice. Treating providers are solely responsible for medical advice and treatment of members. Members should discuss any matters related to their coverage or condition with their treating provider. Health benefits and health insurance plans contain exclusions and limitations.
This is the name of your insurance company and one or more ways to reach them, like their website and phone numbers for customer service or other specific needs. Some of this information may be on the back of the card. Most health insurance cards contain straightforward identification information about the people covered and the policy you have.
But worst of all, I was able to save a list of all my health providers for easy reference which you'd think is great. Well, that is until the app decided to one day delete all my saved providers so that I had to look for them all over again using their terrible search engine and save them again. Who knows how long they'll last in my Saved bucket this time. ACA health insurance offers guaranteed coverage for essential health benefits no matter your medical history. TriTerm Medical Insurance is a short-term health insurance plan designed to last for nearly 3 years,F51 with preventive, doctor office visit, Rx coverage and more. Short Term Medical InsuranceF50 is a budget-friendly health plan for a limited time to help you stay covered when you're between other health insurance solutions.
Network providers help you and your covered family members get the care needed. Access to specialists may be coordinated by your primary care physician. To check if your Oxford Health plan covers therapy, read through your Summary and Benefits document.
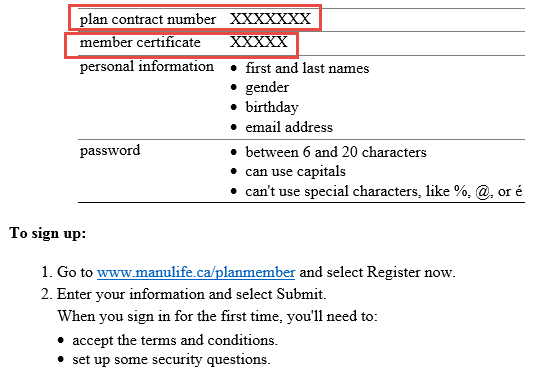
Look for the line that includes "outpatient services" under the "mental health, behavioral health, or substance abuse" category. Oxford Health does not cover therapy services with providers outside of their network — there are no out-of-network benefits. Usually a card's policy number is 8 to 10 digits and can be written in the center. It is helpful to contact your insurance provider if you have any questions. There you'll be able to access information about your plan. Have your health plan ID card ready – you'll need the information to register.
Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. Hi Bernard, thank you for taking the time to read our blog and contact us.
I believe 'pref' is referring to the term 'preferred', which would mean an entity CDPHP has a relationship with and in most cases, gives members access to lower-cost or copay-free services. If your plan includes benefits for prescription drugs, you will also find some information related to them on your health insurance ID card. If you are the policyholder, your name will be on the card. If you have dependents—like a spouse or children—on your health insurance policy, their names might be listed on your card, too. If you are not the policyholder, then your card may show your name and the policyholder's name in separate fields.
To print any page from OSO, simply use the Printer icon in the toolbar at the top of the chapter. A preview window will appear with the correctly formatted pages, minus the site navigation components. Please note that printing restrictions apply – see below for guidelines on legal printing and copyright. From cleanings to root canals, our dental insurance offers plans to help with expenses most health plans don't cover.
Affordable Care Act plans cover preexisting conditions along with a list of essential health benefits. During an ACA Open Enrollment period, you're eligible to sign up for any plans available where you live. Search a directory of network providers, clinics and facilities for Medicare Advantage plans. Also called Medigap, these plans help pay some of the out-of-pocket costs Medicare Parts A and B don't cover. And, you can go to any doctor or hospital that accepts Medicare patients.
Top up online and your key card will be ready to use within 3 hours! Unfortunately products cannot be collected on Stagecoach services at this time. Your health plan ID card is the key that opens the door to your UnitedHealthcare benefits. This link is being made available so that you may obtain information from a third-party website. This link is provided solely as a convenience and is not an endorsement of the content of the third-party website or any products or services offered on that website.
We are not responsible for the products or services offered or the content on any linked website or any link contained in a linked website. We do not make any representations regarding the quality of products or services offered, or the content or accuracy of the materials on such websites. For more information, call UnitedHealthcare Connected Member Services or read the UnitedHealthcare Connected Member Handbook. Benefits and/or copayments may change on January 1 of each year. UnitedHealthcare Connected® (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and Texas Medicaid to provide benefits of both programs to enrollees.
This service should not be used for emergency or urgent care needs. In an emergency, call 911 or go to the nearest emergency room. The information provided through this service is for informational purposes only.
The nurses cannot diagnose problems or recommend treatment and are not a substitute for your doctor's care. Your health information is kept confidential in accordance with the law. The service is not an insurance program and may be discontinued at any time. While it depends on your specific plan, generally health insurance does not cover couples' services. One of the reasons for this is because there is no diagnosis within couples' sessions. Yes, Oxford Health covers behavioral and mental health services within their provider network.
They have an expansive network of mental health professionals that comprise their in-network provider group. Find the health insurance option that is right for you, your family, or your business. As a current member, you can access your benefits and services from your local Blue Cross Blue Shield company.